ICU-metabolism.se © 2010
Publications
Please follow the link to pubmed for all our previous publications.
Recent and older findings, organised from new to old (it has been a while, but now we start again):
September 2023
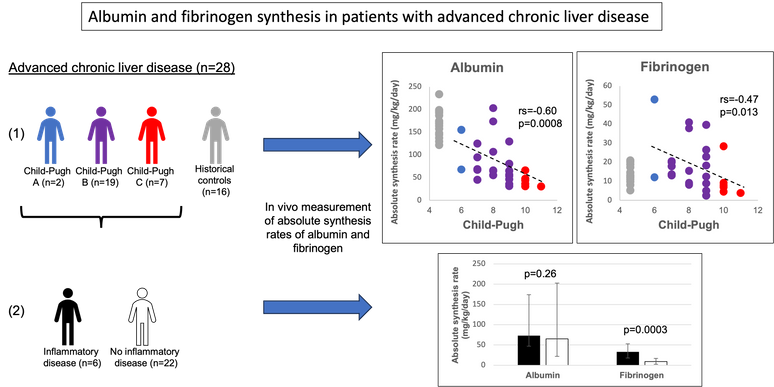
We have just published a paper in which we studies liver protein synthesis capacity in patinets with chronic liver failure. We show that synthesis rates of both albumin and fibrinogen are decreasing with increasing level of liver failure BUT that during inflammation fibrinogen synthesis can be upregulated but not albumin. See graphical abstract below and PDF here.
November 2016 and January 2017
Giving glutamine to ICU patients is controversial since the REDOX study showed a potential for harm. Probably much of this is related to a insufficient knowledge of glutamine physiology during critical illness. We have contributed to the debate with two recent editorials that can be found here and here.
November 2016
In this study we measured albumin levels, albumin transcapillary escape rate (TER) and albumin synthesis rates in patients undergoing major surgery and patients with acute inflammation before surgery. The patients undergoing major surgey had very low albumin levels with an increased TER and an increased albumin synthesis. In the patients with acute inflammation, albumin levels were only marginally decreased and both TER and albumin synthesis rates were normal. Details are here.
November 2016
In an experimental study we investigated whether something in the circulation of critically ill patients could affect mitochondrial function in different organs. To study this, muscle mitochondria and muscle fibres from rats were incubated with plsama from septic patients. The results show that there doesn't seem to be anything in plasma of septic patients directly affecting muscle mitochondria. For details look here.
April 2016
We all know that albumin is low following surgery but it is not really clear when this happens. In this study we performed a detailed mass balance of albumin from anesthesiology start to two days postop in patients undergoing major pancreas resections. The results show that most of the drop of albumin ahppens at the beginning of the surgery; from anesthesiology start to the end of the resection . Details are here.
March 2016
Also in March we published two articles looking into devices to measure energy expenditure in the ICU. In one article two indirect calorimetry devices gave very similar values to the golden standard, the Deltatrac. In the other article a bracelet to estimate energy expenditure was tested as an alternative for patinets in which indirect calorimery is not possible. However the results show that the bracelet is noy better then the Harris-Benedict equations.
March 2016
Some patients in the ICU have very high glutamine levels which is thought to be related to liver failure. In this study we measured plasma glutamine levels in 4 different groups of patients wiith some form of compromised liver function; chronic liver failure, acute liver failure, acute on chronic liver failure and following liver resection. Many of these patients have high glutamine levels but not all. Details in the paper here.
March 2016
From the research group two reviews on nutrition in the ICU were published in the Current Opinion in Clinical Nutrition and Metabolic Care. In these the current knowledge on protein and energy feeding of the critically ill patient are covered. These can be founde here and here.
November 2015
Giving glutamine to ICU patients has become rather controversial since the REDOX trail. However, one interpretation of this is that phamaconutrition, with the intension to upgrade nutrients to phamacological compounds, is not a good idea. On the other hand, this doesn't mean that they are bad as nutrients. One option is that we should only replace glutamine in patients that have a deficit in circulating glutamine. Still there are no studies showing that replacing glutamine in patients with low glutamine levels has a benefit. However, to even consider this option one needs to be able to analyse glutamine levels reasonably fast and preferibly bed-site. However, no devices that do this are available. We have recently validated a bed-site analyser for glutamine that is used for cell culture analyses for analysing circulating glutamine in ICU patients and concluded that it can be used for screeing but not for absilute analyses. For details see paper here.
September 2015
By now we have performed 4 studies within our project on protein nutrition and protein metabolism in critically ill patients. In summary these 4 studies (that can be found below) show that these patients when given protein (either as enteral protein or as parenteral amino acids) utilise the amino acids for improving whole body protein balance without increasing amino acid oxidation as we see in healthy volunteers. A summary figures of a compilation of this data can be found here and are published under Creative Comments license. More details on these here soon.
April 2015 (published April 1st;-))
Lactate levels are often used in the ICU to predict outcome. Especially in acute sepsis or septic shock lactate is used frequently to guide treatment. More and more studies show that the inability of the patient to lower lactate levels is a strong predictor of outcome, even at slightly higher levels. However, there are also patinets with low levels that have a bad outcome and patinets with high lactate levels that survive. A better understanding of the underlying mechanism for the high lactate levels and the inability to lower this is needed. To facilitate this better we validated a 3-pool labelled lactate model to measure skeletal muscle lactate metabolism in humans in more detail. In this study adranaline was used to increase lactate production Results show that the 3-pool model can be used but is due to the large variation and high invasiveness not usefull in all situations and a 2-pool model can be used. The 3-pool model however suggest that the adrenaline induced increase lactate release from muscle is the result of a redirection of a very high lactate turnover intramuscular. In addition we show that adrenaline increases the state 3 respiration of mitochondria in vivo. For all details see here.
March 2015
There is a lot of believe around that critically ill patients need more protein but the proof for this is weak. We have recently published 2 papers that address this issue. In a first paper we study the effect of early low protein enteral nutrition on whole body protein metabolism. For this study we collaborated with Luc van Loon from Maastricht in the Netherlands and used intrinsically labeled milk protein to study this. Results show even this very low dose of enteral protein has a positive effect on protein balance. For all details see here. The second study investigates whether an extra infusion of amaino acids affects protein metabolism in patients with ongoing nutrition. These patients received a 3 hour extra iv amino acid supplementation during the first week of their ICU stay. Results clearly show that this short infusion of amino acids improves protein balance already in the first week of ICU stay. We also observed a very strong correlations between the total protein feeding and the net protein balance, with many patients receiving over 1.2 gram protein/kg/day having a positive protein balance. Article can be found here.
March 2015
In 2012 we published a paper showing that initial glutamine values are predictive for mortality is adult ICU patients. We wanted to know whether this is the same for critically ill children. Fortunately mortality of criticaly ill children is much lower than for adults but this meant that for the study mortality is a probablematic outcome measure. We decided therefore to use orgam failure as the outcome. Organ failue was assessed as a PELOD score. Results show that children with a low glutamine level in plasma when arriving to the pediatric ICU have a higher PELOD score and also have more organs failing. This study opens up the need for glutamien intervention studies also in critically ill children. For all details see here.
December 2014
From a clinical trail that the group performed a few years agao on glutamine supplementation in Scandinavia it was suggested that glutamine supplementation inproved ICU mortality but not post-ICU mortality. This raised the question whether glutamine levels drop fast again after patinets leave the ICU, due to taht the supplementation is stopped, and that this affects the mortality negatively. To investigate this we performed a study to investiga eglutamien levels after teh ICU and whether the post-ICU glutamine levels are related to mortality. Results show that post-ICU plasma glutamine levels are within normal range and are not predictive for mortality outcome. Plasma glutamine level at discharge, on the other hand, is within normal limits but higher in nonsurvivors. In addition, it added prediction value to discharge SOFA scores for post-ICU mortality. For all details see here.
June 2014
Another anesthesiology residents finished his research project recently. Bashar Dabbagh studied the levels of citrulline in plasma of critically ill patients. Citrulline has been suggested as a marker of intestinal function possibly also in the critically ill. Since no good measure for intestinal funstion is available in the critically ill and this is desperately needed, citrulline needs to be validated for this. However little is known about citrulline levels in the crtically ill and Bahar has studies this using 4 older studies with citrulline analyses available. From these studies citrulline levels were studies at admission, the changes in and after ICU treatment and in patients with liver failure. The results show that critically ill patients have low citrulline levels at admission compared to a reference group of young and middele aged healthy volunteers, that the levels on average do not change in and following ICU ward and that liver failure increases citrulline levels. An intereresting observation is that about 20% of all the patients have lower levels then the lowest reference value. The clinical relevance of these finding needs to be elucidated in directly designed studies. For all details see the poster that Bashar produced.
April and May 2014
We have recently published 2 articles on glutamine kinetics in humans. The first one is where we establish the techniques using abolus injection of labelled glutamine and the calculation of glutamine kinetics from the decay of the labelled glutamine in plamsa over 90 minutes. This was done since glutamine has a very large intracellular pool which excludes a steady state of the labelled glutamine when infused continuously. The results from this first study show that the bolus method can be used relaibly, but also that it is very similar to rates measured withe continuous infusion technique. This indicated that both methods measure a rate of apperance of glutamine representing a transport rate through pthe plasma pool. In a second study we used this technique to measure glutamine rate of apperance in critically ill patients in the basel state and during extra glutamine supplementation (as alanyl-glutamine). The results show that the extra glutamine does not inhibit the glutamine rate of appearance, but rather results in a small but significant increase in the rate of appearance. We hypothesize that this is due to the extra amino acids and alanine given at the same time. For all details see the papers here and here.
March 2014
One of the anesthesiology residents finished his research project recently. Imad Almahfoodh studied the effect of lactate changes in critically ill patinets treated in the ICU in Huddinge in relation to mortality. All patients treated in 2013 were screened retospectively and patients with high lactate levels at admission (>3 mM) were inlcuded. Patinets were devided in differemt gropup depending on the time to reach "normal" lacatte levels (<2mM). The results show that patients with a slow or no decrease in lactate have a higher mortality and that this in an independent predictor from APACHE. For all details see the poster that Imad produced.
February 2014
Finally we published our first study on whole body protein turnover in critically ill patinets with MOF. This study was merely to establish the measurements in critically ill patinets to later use it to study the handling of extra parenteral and eneteral protein feeding. In this study we investiagted healthy volunteers fasted and during parenteral nutrition ans show that this results in a anabolic state. We also included 8 patients with MOF. The results show that patients with MOF have a higher protein turnover (both high synthesis and breakdown)andd have a negative protein balance. In addition, we show that the amount of parenteral amaino acids is positively correlated to a positive protein balance. However we used 2 different tracers in this study that gave conflicting results; both showed that parenteral amino acids results in anlbolism but one by increasing synthesis and one by decreasing breakdown. For all details see the paper here.
January 2014
Amino acid metabolism is dramatically changed during critical illness. This is mainly described as changes in plasma concentrations. However, these concentrations in the central circulation are the result of metabolism and feeding (either parenterally and/or enterally). Little is known about the interaction between these and the resulting amino acid profiles. Our research group has published on amino acid levels in plasma during critical illness but the main focus has always been on one amino acid: glutamine. We are however planning to investigate the meaning of the whole amino acid profile more in relation to critical illness and feeding. One of the first studies in this is that we looked at the amino acid profiles in critically ill patinets and how these are related to feeding, length of stay and insulin treatment. This study was doen in collaboration with Greet vanden Berghe's group in Leuven and samples from their large intervention study on intensive insulin treatment nin critically ill children was used for analysing amino acid profiles. The results show that non-surviving children have a higher total amino acid concentratio and that isnulin treatment lowers total amino acid concentration. In addition individual amino acids seem to be related to state of disease, age and insulin treatment. For all details see the paper here.